Male infertility affects 1 in 7 couples globally, and in Pakistan, it is around 21%, making it a surprisingly common challenge. Yet, it often remains shrouded in silence, creating unnecessary stress and isolation for men and their partners. That’s why open communication and seeking help are crucial steps towards successful parenthood.
This guide delves into the different reasons why a man might face infertility, explores the emotional impact on couples, and outlines the support available. Additionally, we’ll discuss how you can optimize your fertility through mindful lifestyle choices and shed light on the various treatment options available to help navigate this journey.
What are the Causes of Male Infertility: A Look Beneath the Surface

Understanding the underlying causes of male infertility is the first step towards finding solutions. Infertility can stem from a variety of factors, often categorized into several distinct domains:
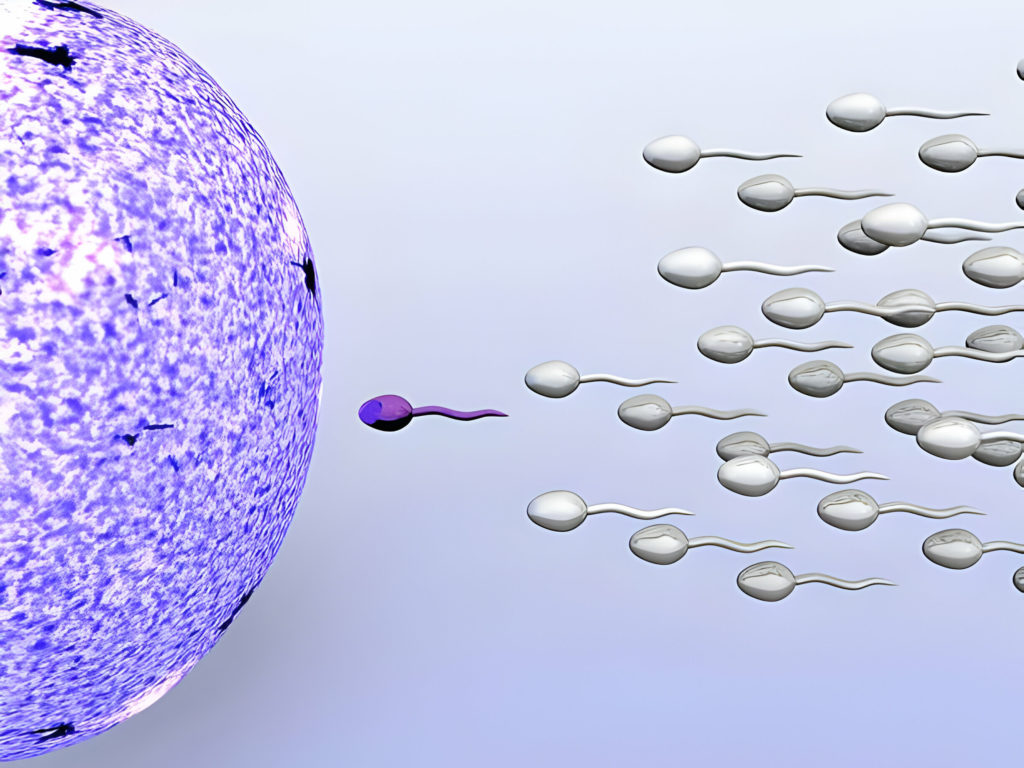
1. Sperm Morphology and Function
Sperm, the microscopic messengers of life, require specific attributes to successfully navigate the female reproductive tract and fertilize an egg. When certain parameters fall outside the optimal range, fertilization becomes less likely. Here are some specific conditions under this umbrella:
- Low Sperm Count (Oligospermia): Sperm production falls below a specific threshold, typically 15 million per milliliter, potentially hindering fertilization.
- Abnormal Sperm Morphology (Teratozoospermia): Sperm deviate from the ideal elongated shape, affecting their ability to reach and penetrate the egg.
- Poor Sperm Motility (Asthenozoospermia): Sluggish sperm lack the vigor to navigate the female reproductive tract, diminishing their chances of success.
These impairments often present without obvious symptoms, highlighting the importance of semen analysis for couples struggling to conceive.
Male infertility ka ilaj chahte hain?
Dr. Farooq Nasim Bhatti se confidential consultation lein aur proven treatment ke zariye apni fertility behtar banayein.

2. Physical Obstacles: When the Path Is Blocked
Sometimes, anatomical roadblocks within the male reproductive system hinder sperm from reaching the ejaculate and embarking on their journey toward fertilization. Here are some specific conditions to consider:
- Varicocele: Enlarged veins in the scrotum trap heat, creating an inhospitable environment for sperm production. This common yet treatable condition often presents without symptoms.
- Retrograde Ejaculation: An anomaly where semen travels backward into the bladder instead of exiting the penis, leaving sperm stranded and unable to participate in fertilization.
- Testicular Obstructions: Blockages within the vas deferens or epididymis prevent sperm from exiting the testicles and joining the seminal fluid. These obstructions can have various causes, including infections, surgery, or congenital anomalies.
Physical obstacles may not always cause noticeable symptoms, making diagnostic evaluation essential for identifying and addressing them. Addressing them through minimally invasive procedures or other interventions can significantly improve the chances of successful conception.
3. Hormonal Imbalances: Disrupting the Orchestra of Fertility
A delicate symphony of hormones plays a crucial role in male fertility. When any member of this orchestra falls out of rhythm, sperm production and quality can suffer.
Here are some key hormonal contributors:
- Thyroid Issues: An overactive or underactive thyroid gland can disrupt the production of hormones like testosterone, which is essential for sperm development and maturation.
- Low Testosterone (Hypogonadotropic Hypogonadism): Declining testosterone levels due to aging or other factors can significantly impact sperm count and motility.
- Other Hormonal Imbalances: Imbalances in hormones like prolactin, FSH, or LH can disrupt the intricate hormonal cascade necessary for proper sperm production and function.
Identifying and correcting hormonal imbalances through medication or other interventions can often restore fertility and allow couples to achieve their dream of parenthood.
4. Genetic Influences: When Nature Holds the Blueprint
In some cases, male infertility can be rooted in genetic factors. While mutations in various genes can impact sperm production or function, some specific conditions deserve mention:
- Klinefelter Syndrome: Having an extra X chromosome can alter testicular development and lead to lower sperm count and abnormal morphology.
- Cystic Fibrosis: The genetic mutation responsible for cystic fibrosis can also affect reproductive health in men, causing blockages in the vas deferens and impacting sperm quality.
Genetic testing can identify these conditions and help couples understand their specific circumstances and make informed decisions about family building.
This is just the beginning of our exploration into the various causes of male infertility. Stay tuned for the next section, where we’ll delve into the emotional impact of this challenge and discuss the range of support available to couples and individuals facing it.
How to Diagnose Male Infertility
Navigating the path towards parenthood and active sexual life when facing male infertility requires a clear understanding of the underlying cause. Fortunately, a variety of diagnostic tools are available to help diagnose the problem and identify treatment options.
1. Semen Analysis
The cornerstone of male infertility evaluation is a semen analysis. This simple, non-invasive test provides valuable insights into several key parameters:
- Sperm Count: Measures the concentration of sperm per milliliter of semen.
- Sperm Morphology: Assesses the shape and size of sperm, which is crucial for their ability to travel and fertilize.
- Sperm Motility: Evaluates the movement and swimming capabilities of sperm, which are essential for reaching the egg.
Results of the semen analysis can point towards conditions like oligospermia, teratozoospermia, or asthenozoospermia, paving the way for further investigation and targeted treatment.
2. Physical Exam
A thorough physical exam by a urologist or other healthcare professional plays a vital role in identifying potential physical contributors to infertility. This exam typically includes:
- Palpation of the testicles: Checking for abnormalities in size, consistency, or tenderness.
- Examination of the penis and scrotum: Looking for signs of varicocele or other anatomical features potentially impacting sperm production or transport.
- Digital rectal exam: Evaluating the prostate gland and seminal vesicles for potential obstructions or abnormalities.
The physical exam allows for immediate identification of conditions like varicocele and can inform further diagnostic steps.
3. Hormonal Spotlight
Hormones play a critical role in directing the symphony of sperm production. Hormone testing helps measure levels of key players like:
- Testosterone: The primary male sex hormone influencing sperm production and maturation.
- Follicle-stimulating hormone (FSH): Stimulates testicular sperm production.
- Luteinizing hormone (LH): Triggers testosterone production by Leydig cells in the testes.
- Thyroid hormones: Affect overall metabolism and can indirectly impact sperm production.
Imbalances in these hormones can contribute to hypogonadotropic hypogonadism or other related conditions, and their correction can significantly improve fertility potential.
4. Ultrasound and Imaging Techniques
Advanced imaging techniques like ultrasound and scrotal MRI can offer a deeper look into the internal structures of the male reproductive system. They can help visualize:
- Testicular masses or abnormalities: Tumors or other structural issues within the testicles.
- Varicoceles and other vascular anomalies: Enlarged veins affecting testicular temperature and sperm production.
- Blockages in the vas deferens or epididymis: Obstructions preventing sperm from reaching the ejaculate.
These imaging techniques provide valuable information for diagnosing conditions like testicular obstructions and guiding surgical interventions if necessary.
5. Exploring Genetic Influences
In some cases, genetic factors may contribute to male infertility. Genetic testing can be used to identify specific conditions such as:
- Klinefelter syndrome: An extra X chromosome leading to abnormal testicular development and low sperm count.
- Cystic fibrosis mutations: Mutations in the CFTR gene can cause blockages in the vas deferens and impact sperm quality.
- Y chromosome microdeletions: Deletions in specific regions of the Y chromosome can affect sperm production or function.
Genetic testing can provide couples with important information and clarify the cause of infertility, allowing them to make informed decisions about treatment options and family planning.
6. Psychological Assessment: Addressing the Emotional Impact
It’s crucial to acknowledge the emotional toll that male infertility can take on individuals and couples. A comprehensive assessment by a psychologist or therapist can explore:
- Depression and anxiety: Common experiences linked to infertility issues.
- Relationship stress and communication challenges: Facing infertility can strain relationships and require open communication.
- Body image and self-esteem concerns: Infertility can negatively impact self-esteem and body image.
- Coping mechanisms and support needs: Identifying healthy coping strategies and accessing appropriate support systems.
Psychological assessment and supportive therapies can help couples navigate the emotional journey of infertility and improve their overall well-being.
By utilizing this comprehensive range of diagnostic tools, including both physical and psychological evaluations, couples facing male infertility can gain a clear understanding of the underlying cause and embark on a targeted treatment path toward realizing their dreams of parenthood.
What are the Treatment Options for Male Infertility
While facing a diagnosis of male infertility can feel daunting, a multitude of treatment options exist. These interventions address the various underlying causes and provide hope and guidance for couples on their journey.
1. Lifestyle Adjustments: Empowering Change Through Health Habits:
Simple yet significant lifestyle changes can often optimize fertility potential in men:
- Diet and Exercise: Adopting a healthy diet rich in fruits, vegetables, and whole grains while engaging in regular physical activity can improve sperm count, morphology, and motility.
- Weight Management: Maintaining a healthy weight can positively impact testosterone levels and overall sperm health.
- Smoking Cessation: Quitting smoking eliminates harmful toxins that damage sperm and impair their function.
- Stress Management: Techniques like mindfulness or yoga can reduce stress hormones that can negatively impact sperm production.
While seemingly minor, these adjustments can significantly increase the chances of natural conception.
2. Addressing Physical Obstacles: Varicocele Treatment:
For cases involving varicocele, minimally invasive procedures can offer significant improvement:
- Embolization: A thin catheter delivers a blocking agent into the enlarged veins, effectively shrinking them and restoring normal testicular temperature.
- Surgery: Traditional surgical options like microsurgical varicocelectomy can also achieve vein blockage and improve sperm production.
Varicocele treatment often leads to significant increases in sperm count and motility, enhancing natural conception potential.
3. Restoring Hormonal Balance: A Symphony of Correct Levels:
Hormonal imbalances can be addressed through targeted therapies:
- Testosterone Replacement Therapy (TRT): For men with hypogonadotropic hypogonadism, TRT restores testosterone levels and can significantly improve sperm production.
- Other Hormonal Interventions: Medications targeting FSH, LH, or thyroid hormones can be used to correct specific imbalances and optimize sperm production.
Restoring hormonal balance can normalize sperm function and pave the way for natural conception or improve success rates with assisted reproductive technologies (ART).
4. Retrieving the Vital Ingredient: Sperm Retrieval Techniques:
In cases where sperm are absent from the ejaculate due to blockages or other factors, specialized techniques can extract them directly from the testicles:
- Testicular Sperm Extraction (TESE): Surgical removal of sperm tissue for use in ART procedures like ICSI.
- Microsurgical Epididymal Sperm Aspiration (MESA): Extraction of sperm from the epididymis, a coiled tube within the testicles, for use in ART.
These retrieval techniques provide valuable options for men with azoospermia (absence of sperm in the ejaculate) to still experience biological fatherhood.
5. Assisted Reproductive Technologies: Joining Forces for Conception:
When natural conception remains elusive, various ART procedures offer viable alternatives:
- Intrauterine Insemination (IUI): Washed sperm are placed directly into the uterus around ovulation, increasing their proximity to the egg.
- In Vitro Fertilization (IVF): Eggs are retrieved from the woman and fertilized with sperm in a laboratory dish, with the resulting embryos transferred back to the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected directly into a mature egg, bypassing sperm transport issues and ensuring fertilization.
These procedures present various pathways to conception for couples facing male infertility, allowing them to build their families regardless of the specific challenge.
6. Exploring Alternative Paths: Adoption and Donor Sperm:
Building a family extends beyond biological possibilities. Couples may consider:
- Adoption: Providing a loving home for a child in need is a fulfilling alternative to biological parenthood.
- Donor Sperm: Using sperm from a carefully screened donor allows couples to experience pregnancy and childbirth and raise a biological child.
Both adoption and donor sperm offer viable and meaningful options for achieving parenthood, enabling couples to experience the joy of family.
The Emotional Landscape of Male Infertility: Understanding and Coping
A diagnosis of male infertility can trigger a complex array of emotions, leaving individuals and couples feeling lost and overwhelmed. Recognizing and addressing these emotions is crucial for navigating this challenging journey.
Coping with the Emotional Storm:
Infertility can lead to a variety of emotional and psychological difficulties for men. Here are some of the common issues that people face in Pakistan:
- Grief, sadness, and frustration: The desire for parenthood may feel unfulfilled, leading to grief for the imagined family and frustration with the situation.
- Feeling like a failure or inadequate: Societal expectations and self-imposed pressures can contribute to feelings of inadequacy and failure, impacting self-esteem.
- Strain on relationships: Open communication and support are vital, but navigating challenges can strain relationships with partners and families.
- Anxiety and depression: The uncertainty surrounding fertility and the emotional burden can lead to anxiety and depression, requiring support and professional help.
Finding Support and Strength:
Fortunately, couples are not alone in facing these challenges. A variety of support systems exist in Pakistan to help them navigate their emotions and find strength:
- Individual and couples therapy: Addressing emotional challenges, communication issues, and coping mechanisms with a therapist can provide valuable support.
- Support groups: Connecting with other couples facing similar experiences can offer understanding, shared experiences, and a sense of community.
- Fertility counseling: At Nasim Fertility Center, Specialized counselors provide guidance, emotional support, and information throughout the fertility process.
Conclusion
It’s important to remember that male infertility is a common issue affecting millions of couples globally. Building awareness and addressing the stigma surrounding male fertility can empower couples to seek help and find the support they need. Remember, you are not alone in this journey, and there is hope for achieving parenthood in its various beautiful forms.
If you are facing infertility Problem, you can Contact Dr. Nasim Farooq Bhatti MBBS, FAACS (USA), Diplomate of the American board of Sexology (USA), CST, HSC (Hong Kong), CART (MALAYSIA), CART (CHINA), Expert Infertility Specialist in Pakistan with over 31 Years of Expereicne.
Disclaimer
This information is for educational purposes and not the treatment. For treatment, you need to consult the doctor.

Dr. Farooq Nasim Bhatti (MBBS, FAACS – USA, Diplomate: American Board of Sexology, CST, HSC – Hong Kong, CART – Malaysia & China) is a qualified medical sexologist with 30+ years of experience. He has presented 21+ research papers internationally and treats sexual dysfunction through sex therapy, counseling, and pharmacotherapy to restore natural sexual function without temporary medication.

Regain Confidence with Our ED Solutions
Explore effective treatments for erectile dysfunction. Take charge of your intimacy today.